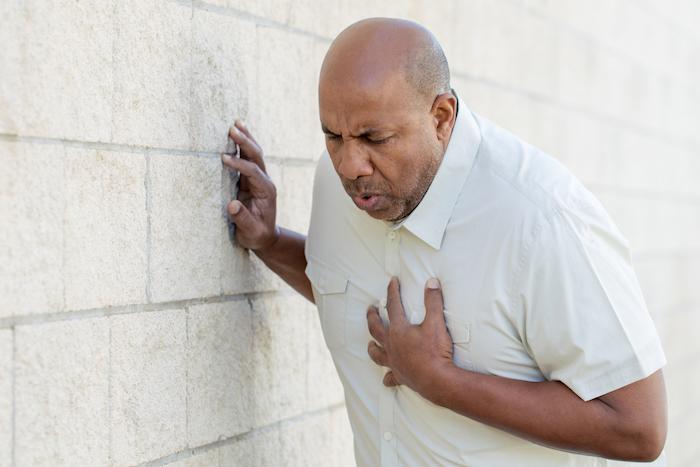
Serious Causes of Chest pain to exclude in the Emergency Department
14th February 2022
5 other causes of chest pain to rule out in the Emergency Department
1st March 2022When a patient is suffering from shortness of breath (dyspnea), it can be very worrying for them and you. Many causes exist, and pinpointing the right issue is sometimes challenging.
Identifying the exact symptoms is essential in coming to the right diagnosis. You need to assess the whole symptom constellation in each patient, perform a general and specific physical examination, and possibly run diagnostic tests.
Here are five serious causes of shortness of breath and some of the differences that can lead to the correct diagnosis.
Pulmonary Embolism
Pulmonary embolism or PE happens when one of the pulmonary arteries in the lungs becomes blocked. It’s usually caused by blood clots and can be life-threatening. Prompt treatment is critical in reducing the seriousness of the condition.
Common symptoms of PE alongside dyspnea include chest pain and coughing. Patients may also experience dizziness, sweating, fevers, clammy skin, and bloody sputum. Tests need to be run to confirm the presence of a pulmonary embolism.
Asthma/COPD
Both asthma and COPD (chronic obstructive pulmonary disease) obstruct airflow from the lungs. These illnesses make breathing difficult and encourage a cough and mucus to surface.
Asthma occurs with the narrowing of the airways, whereas COPD tends to result from long-term exposure to cigarette smoke or other irritating gases. Both can be controlled, but COPD comes with a higher risk of developing more serious conditions.
Patients with either asthma or COPD will need to be observed for frequent monitoring.
Acute LVF
Acute left ventricular failure is apparent when the left ventricle cannot efficiently move blood through the left side of the heart and around the body. This results in a backlog of blood and pulmonary oedema—causing shortness of breath.
Breathlessness usually comes on quickly in these cases and is worse when lying down. Patients will show signs of looking unwell and produce frothy white or pink sputum when coughing. A chest x-ray and ECG can help spot this condition while closely monitoring patients.
Pneumothorax
This term refers to a collapsed lung due to air leaks in the gap between the chest wall and the lung. The whole lung can collapse or just a portion. A chest injury, medical procedure, or underlying disease can cause this issue, but sometimes there seems to be no apparent reason.
Patients will display sudden chest pain and dyspnea. This condition can be life-threatening, and a small needle or chest tube must be inserted to get rid of excess air.
Pneumonia
Bacteria, fungi, or a virus are usually the cause of pneumonia when the air sacs in one or both lungs get inflamed. The condition can be mild to life-threatening and is worse in infants and the elderly.
Look out for other symptoms like chest pain, confusion, fatigue, fever and chills, and nausea. In infants, you’ll notice low energy levels and difficulty eating. Antibiotics are often prescribed to treat the infection causing the condition.
How to make a reasonable diagnosis
While the specific symptoms in clear cut presentations may make the diagnosis obvious in other patients with only a vague symptom of shortness of breath without clear additional symptoms the diagnosis is less clear cut and unless the Emergency Medicine clinician has a high index of suspicion and some experience, significant illness may be overlooked or dismissed as a minor self limiting illness. If such patients are discharged from the Emergency Department and return later with worsening symptoms or critical illness the Emergency Department may face a potential clinical negligence claim.
It therefore is important that the Emergency Medicine clinicians consider these significant diagnoses and positively exclude them before assuming the any shortness of breath is not due to one of these conditions




