Peripheral oedema: When is there a need for emergency or outpatient treatment?
17th August 2022
The Importance of Evidence
30th August 2022Patients presenting with fingertip injuries can be any age with injuries occurring at work or play. The age groups most often seen are the under-5s and the over-65s. The types of injuries most commonly seen include:
- Sharp cuts
- Crush injuries
- Tear injuries
- A combination of all the above
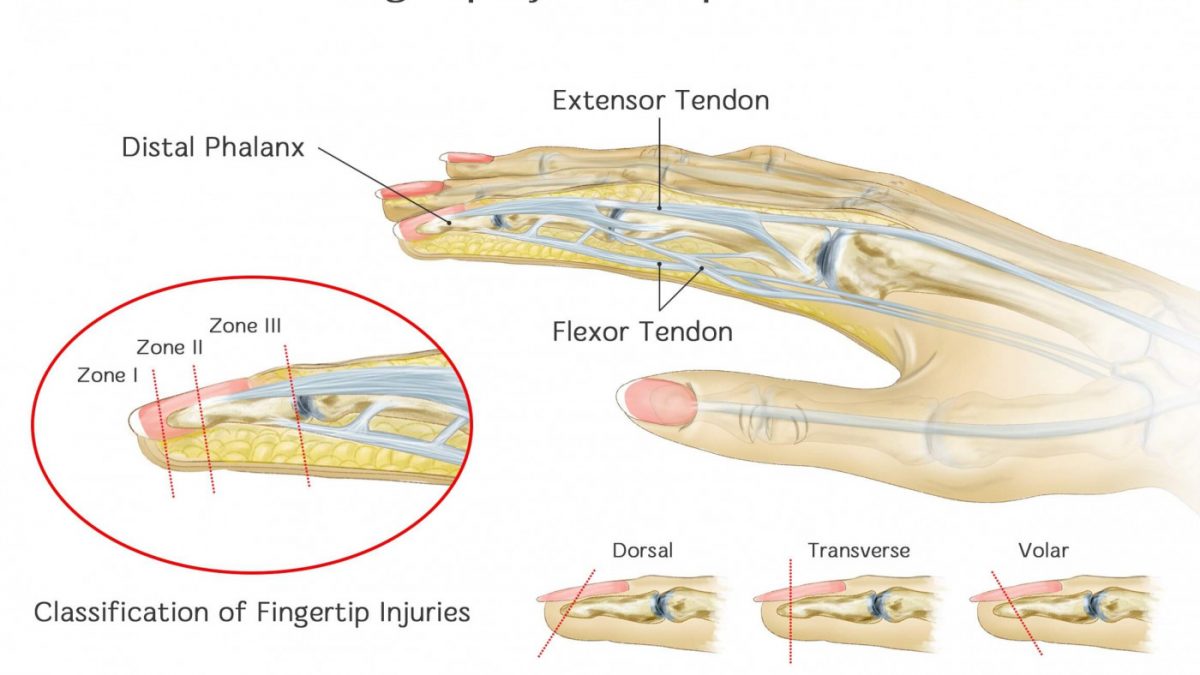
Any part of the fingertip can be injured to include skin and soft tissue, the distal phalanx and/or the nail and nail bed. It is very common to see partial (where some structure remains) or complete (where the whole fingertip is gone) amputations of the fingertip.
Treatment goals
The main aims in treating fingertip injuries are restoring sensation and viability of the fingertip and ensuring enough bone support for nail growth to maintain the normal appearance of the finger.
Where fingertip amputations are not treated properly and expeditiously this can result in defects such as hook nail deformity and more importantly can result in excessive tenderness of the skin with intolerance to cold temperatures and possible long-term loss of function.
Presentation and diagnosis
Laceration, avulsion and compression are the types of injuries which most commonly present in the ED with sometimes accompanying subungual haematomas. There is commonly a great deal of pain with these injuries and especially where the nail has been torn from the nail bed.
Compression of the nail bed plus fingertip amputation may be the result of a heavy or sharp object and injuries can range from distal phalanx fracture to partial or complete amputation of the tip. Children are the ones who most commonly present with this type of injury from an accidental door closure on the hand. Detailed information about the nature of the injury should be collected.
The injury should be examined manually to assess the residual function and sensory feeling of the fingertip. A light touch sensation test and examination of the colour and capillary refill of the finger should assess the vascular capacity and function of the finger. At the same time you should look for any foreign bodies including metal, wood or glass. If a fracture or dislocation is suspected, demonstrated by the amount of pain shown, anterior, posterior, lateral and oblique x-rays should be taken.
Treatment and management – Loss of Volar vs Dorsal Skin Amputation vs Reconstruction
Treatment will depend on the range of the amputation (transverse or oblique) of the fingertip and the type of skin (vascular and sensory function) involved (volar or dorsal).
Non surgical management with simple dressings and painkillers can be utilised to promote secondary healing. These patients usually heal quickly with no loss of motor function.
Where there is less than 2cm of skin loss and no loss or exposure of bone or tendon, a wound may be left open to heal by granulation and the patient should be advised on the appropriate type and duration of wound dressing. This treatment has been proven to aid full recovery with no loss of normal function.
A surgical team referral is needed in cases of severe fingertip amputation. Surgery to trim any protruding or damaged bone and tissue may be necessary. This may entail some loss of skin, nail and finger length. Fill thickness skin grafting or flap reconstruction may be necessary in some cases.