Allergies in the Emergency Department
27th April 2021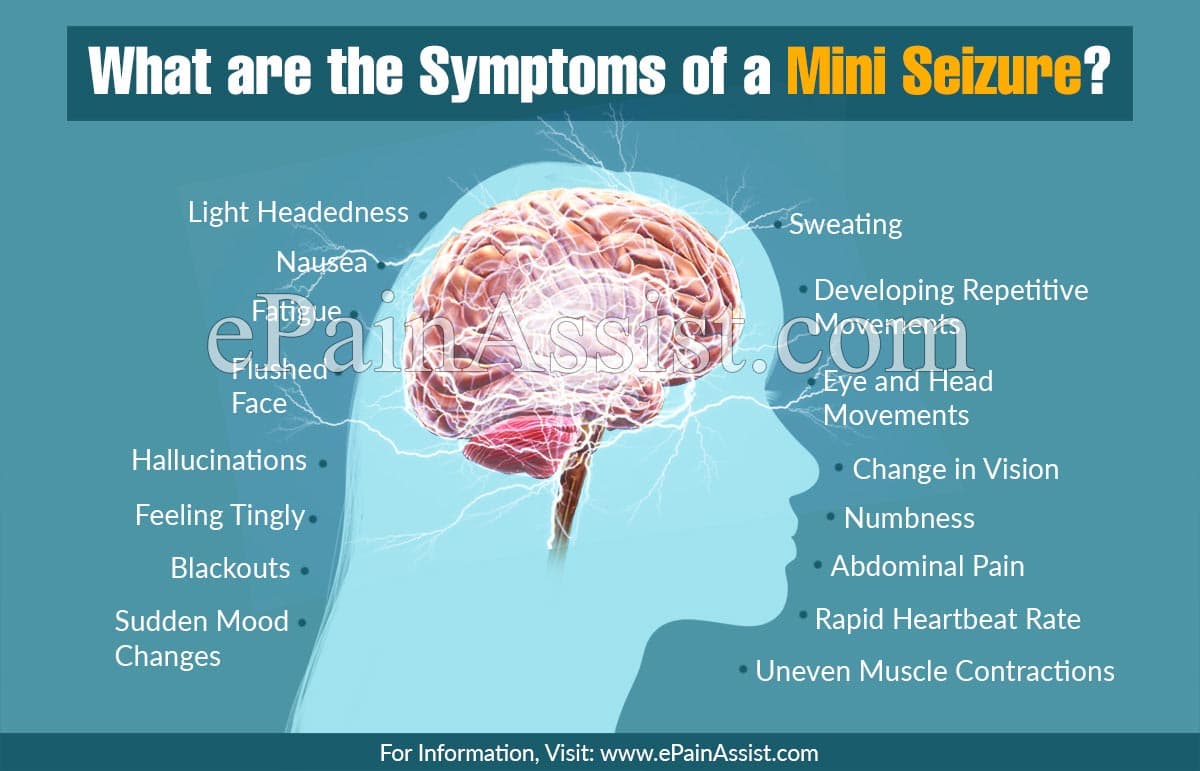
6 Key Factors to Observe in Unexplained Seizures
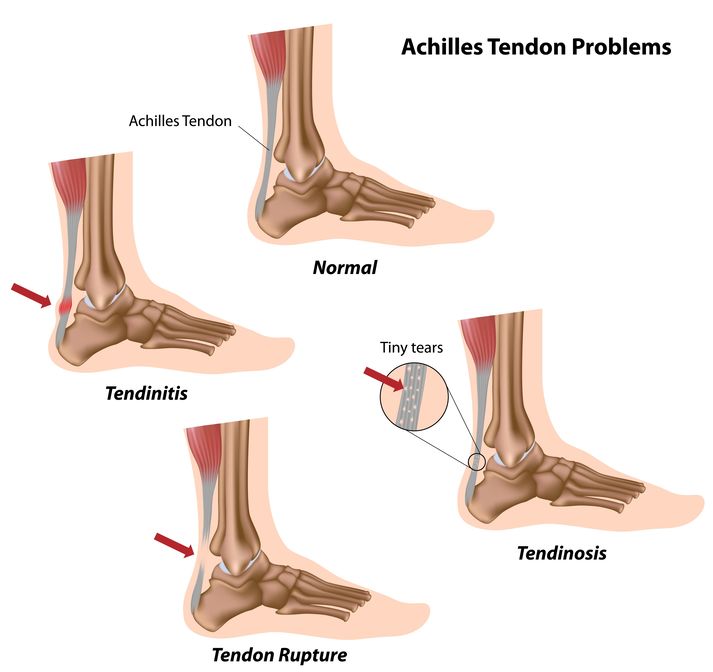
19th May 2021The Achilles tendon (or calcaneal tendon) is the strongest tendon in the body and connects the soleus and gastrocnemius muscles to the calcaneal (heel) bone. Despite this tendon being extremely thick, overuse and damage is quite common, especially in sports-related injuries.
Ruptured Achilles tendon
The Achilles tendon may rupture when the foot or ankle undergoes a sudden force trauma, especially during sports such as football, causing instant difficulties for the patient who will lose the ability to plantar flex, consequently causing an abnormal gait. As expected, pressure on the affected foot will be painful.
An Achilles tendon rupture often occurs when a tear in the tendon fibres can lead to a full or partial tear of the tendon. A typical presentation of this type of injury would be when the patient describes hearing a “popping” sound coming from the back of their heel or calf area. Often people say they felt like someone kicking them in the heel.
A tendon rupture requires immediate medical attention and needs to be assessed by a medical professional.
Achilles tendonitis
The second type of Achilles tendon injury is tendonitis or tendinopathy. Tendonitis is typical caused by impact damage to the area or simply due to wear and tear over time and is very common in athletes.
There are two types of achilles tendonitis:
Insertional Achilles tendonitis when damage occurs to the tendon around the heel bone, and there could even be extra bone growth with this type of tendonitis.
Non-Insertional Tendonitis describes the process when small tears in the middle fibres of the tendon cause it to deteriorate, resulting in noticeable pain and swelling. This is a typical injury that is seen amongst fitter and younger adults.
Specific symptoms for tendonitis include pain down the back of the leg or around the heel area. The patient may have difficulty moving the affected joint and may even feel grating when moving the tendon.
Tendonitis requires immediate treatment as the injury may worsen over time, leading to a ruptured tendon.
Diagnosing achilles tendon injuries
A common issue with this type of injury is that it can be misdiagnosed as a sprained ankle – a thorough diagnosis must be carried out so that the clinician can carry out the right corrective action.
A comprehensive review of the symptoms needs to be carried out. The emergency department clinician should complete a physical examination of the Achilles tendon to check for swelling, painful areas, and evidence of bone spurs. This is especially effective for diagnosing Achilles tendonitis.
The Thompson test is a standard test used to identify the presence of a complete Achilles Tendon Rupture and is performed by squeezing the calf. A Matles test is the reverse of a Thompson Test but can also diagnose a ruptured Achilles tendon by looking for exaggerated foot drop when the knee is flexed.
The patient can also be asked to stand on tiptoes and if the Achilles tendon is not intact this is not possible
Treatment for achilles tendon injuries
Treatment for Achilles tendinitis is straightforward. Prescribing rest, ice and support should aid in a full recover. A referral to physiotherapist may also prove necessary for taping and other musculoskeletal support. Administration of NSAIDs may also occur to reduce swelling.
For an Achilles tendon rupture, younger patients often undergo surgery to repair the rupture whilst older patients prefer non-surgical treatment. Surgery involves stitching the torn tendon together although one of my previous bosses said that it may be like stitching 2 shaving brushes together . Non-surgical approaches include resting the tendon often in a plaster in equinas ( the foot extended downwards) on crutches, applying ice and NSAIDs for inflammation. Patients are advised to wear shoes with heels to ensure the foot is kept flexed during recovery.