Expert Witness Error in Family Court: A Warning for Medico-Legal Professionals
29th May 2025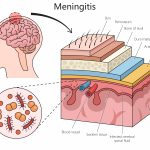
WHO Releases First‑Ever Global Clinical Guidelines on Meningitis: Legal and Ethical Implications for Medico‑Legal Practitioners
26th June 2025Hyponatraemia, is described when a serum sodium concentration is below 135 mmol/L. It is one of the most common electrolyte disturbances encountered in clinical practice and ranges in severity from mild and asymptomatic to life-threatening, with symptoms such as confusion, seizures, coma, and death in acute or severe cases. Despite its frequency, the management of hyponatraemia requires meticulous attention to both the underlying cause and the rate of correction, as overly rapid correction poses significant clinical and legal risks—particularly the risk of osmotic demyelination syndrome (ODS). For medico-legal professionals, understanding the nuances of hyponatraemia and the implications of clinical mismanagement is crucial for evaluating potential negligence or malpractice.
Clinical and Legal Implications of Hyponatraemia Management
Hyponatraemia may be acute (developing in <48 hours) or chronic (>48 hours), and the distinction is central to determining the appropriate management strategy. Acute hyponatraemia may warrant more aggressive correction due to the risk of cerebral oedema. In contrast, chronic hyponatraemia requires a far more cautious approach, as the brain has already adapted to the hypotonic environment by reducing intracellular osmolytes. Rapid correction in these patients can cause water to move too quickly out of brain cells, leading to cellular dehydration and demyelination, particularly in the central pons.
The most feared consequence of overly rapid sodium correction is osmotic demyelination syndrome (ODS), formerly known as central pontine myelinolysis. ODS can present with a range of debilitating neurologic deficits, including dysarthria, dysphagia, quadriparesis, locked-in syndrome, and even death. These deficits are often irreversible, resulting in profound and permanent disability, which carries significant medico-legal ramifications if the condition arises as a consequence of iatrogenic mismanagement.
Guidelines and Legal Standards
Clinical guidelines from international authorities such as the European Society of Endocrinology and the U.S.-based Endocrine Society recommend that the serum sodium correction rate in chronic hyponatraemia not exceed 8–10 mmol/L in 24 hours and 18 mmol/L in 48 hours. For high-risk patients, such as those with alcoholism, malnutrition, or advanced liver disease, even more conservative targets—such as ≤6 mmol/L per 24 hours—are advised.
From a medico-legal standpoint, these guidelines can serve as standards of care. A clinician deviating from these established thresholds—especially without clear documentation of the rationale—may be exposed to legal liability if the patient subsequently develops ODS or related complications. Courts may view such a deviation as a breach of duty if it falls outside the practice accepted by a responsible body of medical opinion and leads to harm.
Common Pitfalls and Legal Risks
Legal claims related to hyponatraemia often arise not from the failure to diagnose the condition, but from the failure to appropriately manage it. Common medico-legal pitfalls include:
- Inadequate Monitoring: Failure to frequently monitor serum sodium levels after initiating correction can allow unrecognized rapid rises.
- Incorrect Fluid Administration: Use of hypertonic saline without careful calculation of the desired correction can result in overshooting target levels.
- Failure to Re-lower Sodium: Once an overcorrection is identified, failure to implement re-lowering strategies (e.g., desmopressin and free water) can compound harm.
- Insufficient Documentation: Lack of documentation regarding the estimated duration of hyponatraemia, risk stratification, or justification for management decisions weakens the legal defense in case of complications.
Conclusion
Hyponatraemia, while common, is not benign when mismanaged. The consequences of rapid sodium correction are severe, irreversible, and often legally actionable. For clinicians, strict adherence to evidence-based guidelines, vigilant monitoring, and comprehensive documentation are not only good medical practices—they are essential legal safeguards. For medico-legal professionals, awareness of these clinical standards is key to assessing liability in cases involving neurologic deterioration after sodium correction. In an era of increasing scrutiny over patient safety, even small deviations in electrolyte management can carry outsized legal consequences.