Chasing Changing Guidelines
20th April 2020
Expert Struck off – A salutary lesson
28th April 2020Imagine this scenario: A patient attends the Emergency Department with a wrist injury and after assessment and X-ray is reassured and discharged. After experiencing prolonged pain and stiffness in the wrist, the patient receives a further X-ray that reveals an un-united fracture of the scaphoid, which prompts them to initiate a claim for a missed diagnosis.
The problem
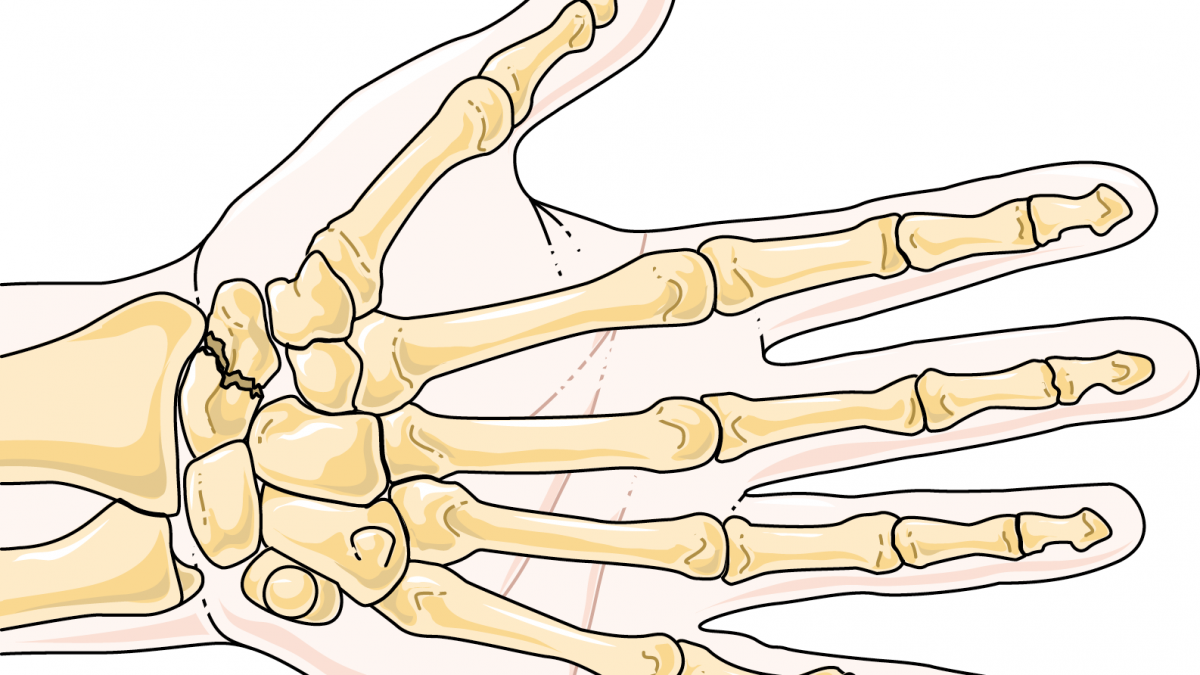
The scaphoid is a small bone on the thumb-side of the wrist. An injury to this bone is unusual in that a fracture may not be visible on an X-ray taken immediately after the injury and may only become visible on an X-ray taken 10-14 days after the injury.
When a fractured scaphoid is suspected, the standard treatment is to immobilise the wrist and then re-assess and X-ray the patient after the required period of time has passed.
The clinical signs
A number of clinical signs have been used to make a diagnosis of a scaphoid fracture but in 2013, the Royal College of Emergency Medicine RCEM produced a guideline indicating that either tenderness in the anatomical snuffbox (the hollow between the tendons on the thumb-side of the wrist) or over the scaphoid tubercle (the palmar surface of the scaphoid) should be an indication of a scaphoid fracture even if the X-ray was normal.
However, while one or both of these symptoms would be found in more than 90% of scaphoid fractures, only 30% of those experiencing only one of these symptoms have a diagnoseable fracture. A meta-analysis on adult scaphoid fractures conducted by Carpenter et al. (2014) confirms that the absence of anatomical snuffbox tenderness, scaphoid tubercle tenderness, or pain on telescoping the thumb reduces the possibility of a scaphoid fracture. The study also indicates that treating all of the patients with one or more of these symptoms would mean that for each patient with a true scaphoid fracture, four patients would be unnecessarily immobilised awaiting further diagnosis.
The expert opinion
Whether a patient had a scaphoid fracture upon presenting to the Emergency Department is a matter not for the expert to decide but for the court. The expert’s job is to evaluate whether the initial clinician carried out the correct investigations and treatment when assessing the injury. It is not within the expert’s role to diagnose the patient in retrospect.
In my opinion, if the court determines that the patient had a scaphoid fracture, then on balance of probabilities a reasonable examination would have found one or more of the clinical findings to be present and therefore the patient treated as though they had a fracture.
However, based on the clinical guidelines outlined above, if the patient did not have a fracture it would be reasonable for there to be no positive signs. If the court determines that then failing to find positive signs would be reasonable.




3 Comments
[…] Previously, I talked about the scaphoid fracture and how this can be missed in the Emergency Department. […]
[…] C-spine injury exists, through a process called “clearing the cervical spine.” As discussed in previous posts, clinicians often need to balance an accurate diagnosis with safely decreasing the patient’s […]
[…] complex, which is why fractures and other injuries can be easy to miss, even with radiographs. (See my past article on scaphoid fractures.) This underscores the importance of a clinician’s physical examination skills and the ability to […]