
Why An Expert Witness Needs A Website
9th March 2021
Managing the pregnant patient in the Emergency Department
25th March 2021Patients often present to the Emergency Department having been out (when the pandemic allows) and having taken intoxicating drinks. They may have fallen and injured their hands with glass or have been involved in assaults with glass or knives.
The key injuries that the Emergency Clinician has to exclude are those to the nerves or tendons of the hand. Both of these in the normal assessment process require the cooperation of the patient for examination – but those who are under the influence may not understand why they need to cooperate and may give equivocal answers to questions.
Asking the patient to return for a second assessment when they are sober may not be easy and the patient may not remember the instructions to return, thus leading to a possible delay in diagnosis and treatment leading to claims of clinical negligence.
There are however some ways that the examining clinician may be able to test for nerve or tendon injuries in a non-cooperative intoxicated patient.
The nerves supplying the hand are either mixed sensory and motor nerves or just sensory nerves. All sensory nerves carry sympathetic nerve fibres that cause the areas they supply to sweat. If the nerve is cut, loss of sensation the skin may occur and the skin could lose sympathetic feedback, becoming dry due to a lack of sweat production.
Sympathetic nerve injury can be tested objectively with a test known as tactile adhesion. This is best done with a Bic Pen, drawing it across the skin. Normal skin has slight resistance to the pen whereas skin where the sensory nerve is divided provides resistance and then slides across the skin.
To check if the tendons are intact without a cooperating patient who has moving fingers, the clinician can use the fact that the tendons are of fixed length and passive movement of the wrist causes the finger tendons to alter position, even without active participation. If the wrist is extended (bent back) the fingers automatically bend and when the wrist is flexed (bent forwards) the fingers straighten.
If a tendon is completely divided, the finger with the injured tendon will not function properly. In a flexor tendon injury (the tendons that bend the finger), the finger remains straight while the others bend (the pointing finger sign). If the tendon is only partially divided there may be movement on undertaking this test but it will identify the more serious injuries and even if an injury identified later recording that an examination had taken place this would be within a reasonable standard of care.
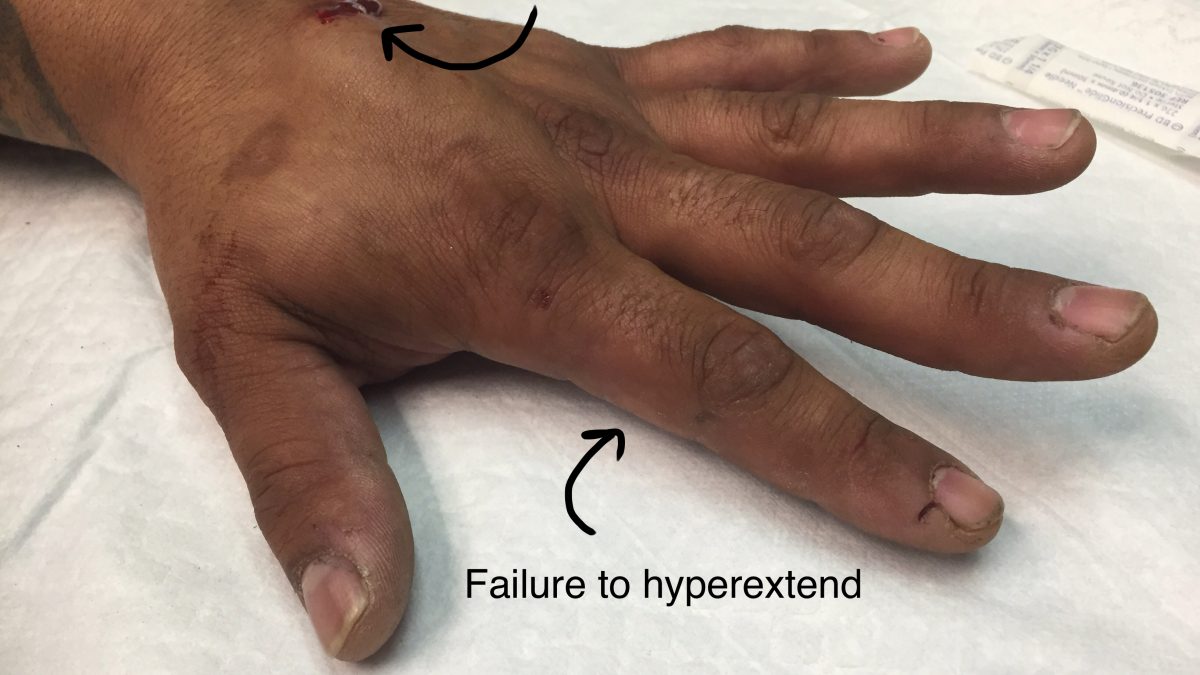
An extensor tendon injury is a more common injury found in intoxicated patients. The extensor tendons allow either the wrist, hand or finger to straighten. An extensor injury is indicated if the patient struggles to straighten their finger to thumb without pain. A cut across the back of the hand or finger will suggest that this injury has occurred.



1 Comment
[…] a patient’s history is key, otherwise speed in delivering appropriate treatment if you don’t know the cause or it […]