Cardiac Arrythmias Defined
3rd May 2022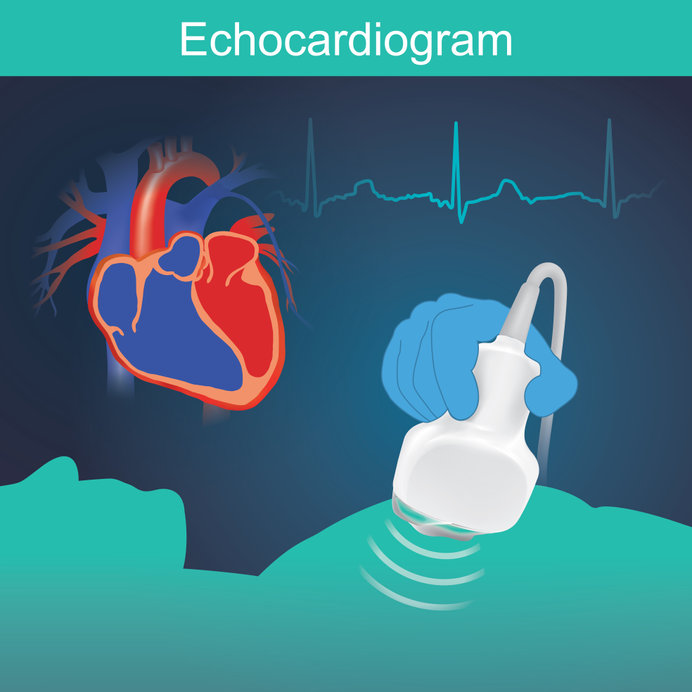
The emergency treatment of Cardiac Tamponade
18th May 2022Tachycardias can range from those that are life threatening through those causing major cardiovascular instability to those with minor symptoms for the patient.
Having established by clinical examination that a patient has a rapid heart rate the first differentiation is whether on an ECG the trace looks like a normal heartbeat but rapid or is the form of the electrical trace is abnormal and wider than normal.
This leads to either the patient requiring treatment for a narrow or broad complex tachycardia.
Broad complex tachycardias originate mainly in the ventricles and so are called ventricular tachycardias. Untreated, this condition could sometimes cause sudden cardiac death. The goals of treating ventricular tachycardia in an emergency setting are to slow the rapid heartbeat and prevent future episodes
Narrow complex tachycardias can come from a variety of sources but all start above the ventricles such as , atrial tachycardia, AV-nodal re-entrant tachycardia or tachycardia caused by accessory pathways, the characteristics remain similar, with a ventricular heart rate of greater than 100bpm and small QRS complexes with widths of equal to or less than 0.12 ms.
It’s essential to correctly evaluate the patient’s history, perform a full physical exam, and ensure the electrocardiogram is properly analysed although in the Emergency Department this can be aided by automatic interpretation by the ECG machine. If this is done, over 90% of cases can be precisely diagnosed.
Should another condition be to blame for tachycardia that is the rapid heart rate is due to for example blood loss, it’s essential to treat the underlying problem in order to reduce or prevent future episodes.
Treating Tachycardia in an emergency setting
When it comes to acute treatment of SVT an ECG should be performed as soon as it is possible to do so.
The patient should be assessed to determine whether they are haemo-dynamically stable or unstable.
If the patient is haemo-dynamically unstable the most effective way if stopping tachycardia is via direct current cardioversion This can work for both ventricular and supraventricular tachycardia with the latter being undertaken with the shock synchronized to the ECG tracing
Should the patient be haemo-dynamically stable, there are various options:
For regular narrow QRS complex tachycardia in haemo-dynamically stable patients, vagal manoeuvres including carotid massage, facial immersion in cold water and Valsalva may be used.
Carotid Massage
It should be noted that carotid massage is usually used primarily in younger patients. It is important to auscultate for bruits prior 2 performing carotid massage, to lower the risk of stroke from emboli and not to perform message on both sides at the same time.
Valsalva
In anywhere from 5 to 20% of patients, this manoeuvre may induce cardioversion. There is a modified manoeuvre, where the patient is laid flats with their legs elevated once the strain phase is completed. This was shown in a randomised controlled trial to increase the success of cardioversion to more than 40%.
Medication
Should manoeuvres fail, IV adenosine or verapamil could be given. However, it’s essential that resuscitation equipment is on hand in case the patient experience ventricular fibrillation or bronchospasm. Other consideration include whether the patient has severe asthma. If so, adenosine IV may not be the most appropriate choice due to high incidence of side effects such as chest tightness and shortness of breath. In such case, IV verapamil could be a more appropriate choice. Oral beta-blockers could be useful for emergency treatment of AVNRT, such as diltiazem or verapamil.
Should the above manoeuvres and medications fail, or they are contraindicated, then treatment must be via DC cardioversion.