Paracetamol overdose: how to avoid medical negligence claims
2nd April 2021
Fellow of The Expert Witness Institute
19th April 2021Diabetic patients have difficulty maintaining normal blood sugar levels and can result in medical emergencies if uncontrolled. It is a useful pneumonic to remember that after assessing and checking the ABC’s ( Airway Breathing Circulation) that the DEFG can remind the clinician to Don’t Ever Forget Glucose and check the patients blood sugar level.
Diabetics attending the Emergency Department with altered conscious levels could be suffering from either hyperglycaemia ( high blood sugars) or hypoglycaemia ( low blood sugars). While a rapid glucose level may be easily obtained to allow correct treatment to be started if it cannot the risk of giving a hyperglycaemic patient glucose is less than the benefit of giving it to a hypoglycaemic patient as the brain relies on glucose to maintain normal function.
If a patient who normally has good control of their blood sugars attends the Emergency Department and their Glucose levels are outside their normal pattern then it is important for the clinician to look for reasons that could cause this such as other illnesses that need diagnosis and specific treatment rather than simply altering the normal glucose regime.
For a hyperglycaemic crisis, consider the 5Is: infection, infarction, infant (pregnancy), indiscretion (cocaine use) and insulin deficient (either due to incorrect dosing or nonadherence). (Ford et al., 2013) If the patient has diabetic ketoacidosis (DKA), an insulin bolus should be administered. A fingerstick glucose test should be performed every hour to monitor restabilisation.
DKA occurs when the body overproduces ketones in response to a build-up of glucose in the blood and is most often seen in Type 1 diabetics. A combination of ketones and glucose is lost in the urine and causes severe dehydration. More serious symptoms develop as a consequence, namely cerebral oedema, resulting in a coma and brain injury.
The main goals for the Emergency Department in reversing DKA is (1) restoring fluid balance with saline, (2) replacing potassium (a common complication of DKA) and (3) reducing the blood sugar level with controlled insulin infusions
For hypoglycaemia, blood sugar levels will be below 4 mmol/litre. In severe hypoglycaemia, transient neurological changes can occur. This includes convulsions, paresis, encephalopathy and in worst case scenarios, subsequent neurological damage. The patient may also be unconscious.
As stated above because of the seriousness of this condition urgently giving a glucose bolus is the treatment of choice if the patient is unconscious but if the patient is co-operative with a low blood sugar and can swallow safely giving glucose gel is an alternative and has the advantage that the 10% glucose solution can irritate the veins and using oral gucose can avoid this complication.
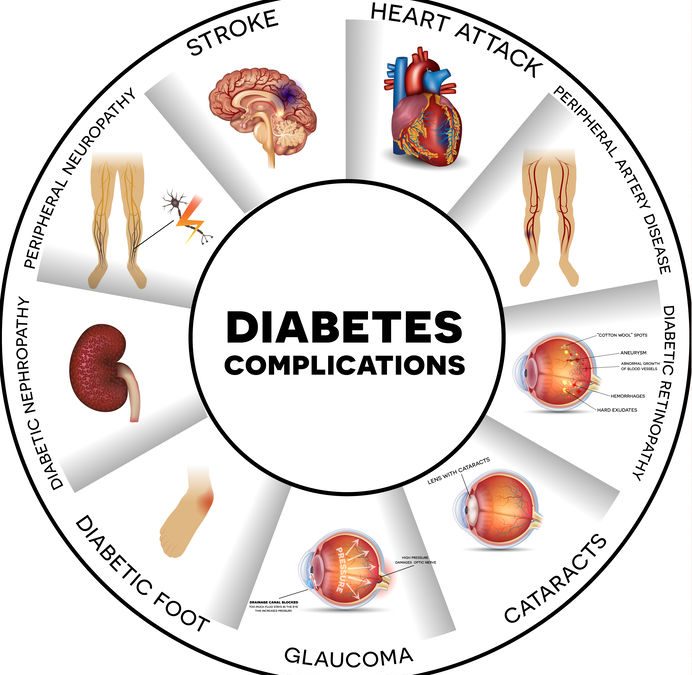
Long term complications of diabetes
With the length of time a patient is diabetic they run the risk of developing complications due to damage to the microvascular system that is the small blood vessels in the body.
This can be seen in the blood vessels on the eyes and can cause the patient ot present ot the Emergency Department with altered vision. In most of these circumstances such patients do not need emergency treatment but should be referred ot an ophthalmology clinic for further treatment.
Much more common is the diabetic patient presenting with foot problems often with infections of the feet or ulcers on the feet. The patient may not even have been aware of the development of changes in the feet as not only are the blood vessels damaged but there is also damage to the nerves leading to altered sensation or numbness in the feet.
While assessing the patient in the Emergency Department it is useful to check all the pulses in the lower limbs in contrast to patients presenting with peripheral vascular disease where changes in the feet are usually accompanied by alteration in the pulses in the groin or knee patients with diabetic foot problems may have clinically normal pulses in the legs but changes or ischaemia or gangrene in the toes.
The patient may present late as they may not notice that for example their footwear is pressing against skin that is numb leading to pressure and ulceration on the toes.
When the patient has such changes and any infection does not settle with the normal antibiotics consideration as to whether they are developing osteomyelitis ( infection in the bone) must be excluded by an X-ray.
Most hospitals have a diabetic foot service where these type of problems are seen by a multi-disciplinary team and while the Emergency Department may not have immediate access to such a service they should inform the patient’s GP that referral to such a service may be important for long term management of the patient and preventing further complications and repeated attendances at the Emergency Department.
Diabetes is becoming a common disease in the population and the Emergency Department sees both patient with consequences of the blood sugar disturbances themselves but also the complications from that disease.
Simple tests such as a finger prick test can help the clinician manage the acute problems but it is important that the Emergency Department signposts to the patient and their GP how this disease may need long term management and the referral to appropriate specialist services.




1 Comment
[…] The GIRFT New Pathway provides support for NHS teams at the ‘front door’ to enable better care and support for patients who present in EDs with diabetes and/or hyperglycaemia and other issues relating to a previous or new diagnosis of diabetes. Interactive versions of the GIRFT Pathways are now available to clinicians outlining the exact processes and decision-making channels they need to access in order to follow best practice guidelines and provide the best care and outcome for the patient. The Pathways relate to the management of patients presenting in the ED with a foot problem, or with hyperglycaemia or hypoglycaemia. […]