The emergency treatment of Cardiac Tamponade
18th May 2022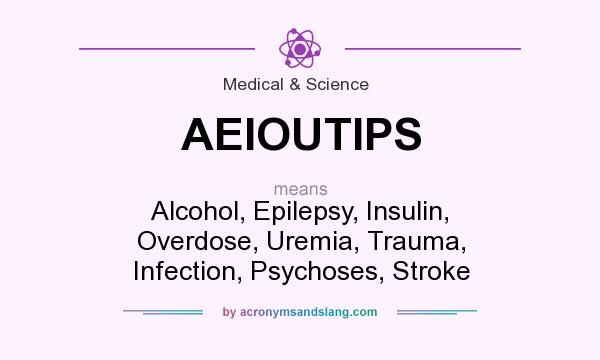
AEIOU TIPS – What are the common causes of unconsciousness in the emergency department?
7th June 2022Febrile convulsions most commonly occur in children between the ages of 6 months to 6 years. A typical seizure will normally last between 2-3 minutes and rarely more than 10 minutes.
A seizure typically presents as a generalised tonic- clonic type – that is the muscles stiffening followed by the rhythmic shaking or jerking of the limbs. This may be asymmetrical in presentation. Other symptoms to be aware of when looking to make a diagnosis include twitching of the face, including a rolling back of the eyes and also a loss of consciousness. Look for foaming of the mouth, a difficulty with breathing, pallor of the skin or cyanosis.
During the period following a febrile convulsion seizure the patient will experience a brief post-ictal period of drowsiness, confusion or irritability. Complete recovery should be seen within 1 hour. It is important to ascertain if the patient has previously experienced a febrile seizure when taking a medical history.
A complex febrile seizure will include one, or more, of the following features:
- Seizures last over 15 minutes
- There is a recurrence of seizure within a 24 hour period or within the same febrile episode
- Recovery is incomplete within 1 hour and may include transient hemiparesis (Todd’s palsy) or prolonged post-ictal drowsiness
- There may be focal features or partial onset (typified by movement that is limited to one limb or one side of the body)
Assessment
The patient should be assessed for any red flag signs and symptoms – encephalitis, meningitis/meningococcal disease, and those conditions that mimic a febrile seizure. Assessment should include noting if there was a fever, including when it started, duration and peak temperature. When the fever occurred in relation to the seizure. Post-ictal drowsiness duration, any recent antibiotic use and any recent immunisation history should also be noted along with a neurodevelopment history, including any concerns, and family history of epilepsy or febrile seizures.
A full examination of the child should include assessing consciousness level, checking temperature, checking for dehydrations and all other signs that might identify underlying causes for febrile illness. In some cases blood glucose and urine dipstick analysis may be appropriate tests to order to assist with further diagnosis or exclusion of certain conditions.
Management
The majority of children attend a medical setting following a febrile seizure. Simple first aid measures such as removing clothing down to a nappy or pants may reduce the temperature and prevent a second seizure. Giving antipyretics such as paracetamol or Ibuprofen is also recommended. An immediate assessment should be arranged in order to determine whether the cause of the seizure was something that needs specialist medical treatment (encephalitis, meningitis/meningococcal disease).
Advice and education to parents or carers should be provided and reassurance given that febrile seizures are not the same as epilepsy, nor do they increase risk of developing epilepsy. Information on further sources of information should also be given including information on recognition and management of possible future episodes. In some cases following a specialist assessment Benzodiazepine rescue medication may be prescribed for future use. Appropriate follow up care should also be arranged where it is deemed necessary.
Advice on OTC medication for the reduction of temperatures, stripping the patient as above if they develop a temperature from a viral type illness may also prevent recurrence if there is no other cause found for the convulsion after assessment in future and on keeping hydrating may also be appropriate.




