Nurrish v Nursing and Midwifery Council: A Cautionary Tale in Remote Fitness to Practise Proceedings
12th February 2026The distinction between infection and sepsis is fundamental in clinical medicine and has major medico-legal consequences. Although the terms are sometimes used interchangeably in casual discourse, they represent markedly different clinical states. In medico-legal practice, failure to recognise when a patient has progressed from infection to sepsis is a recurring theme in negligence claims, inquests, and regulatory investigations.
Defining Infection
An infection occurs when pathogenic microorganisms invade the body and cause a host immune response. Infections may be localised or systemic but remain physiologically contained.
Typical features include:
- Local or mild systemic inflammatory response
- Symptoms related to the site of infection
- Preservation of organ function
- Clinical stability
Common clinical findings may include fever, localised pain or inflammation, dysuria, cough, or mild tachycardia. In uncomplicated infection, the host response is proportionate and effective, homeostasis is maintained, and patients usually respond to routine treatment.
From a medico-legal perspective, the presence of infection alone does not imply negligence. It also doesn’t necessarily require urgent escalation provided the patient remains stable and appropriately monitored.
Defining Sepsis
Sepsis is a life-threatening condition arising from a dysregulated host response to infection resulting in acute organ dysfunction. It is defined as different to an infection as a disease process to instead, systemic physiological failure.
Key characteristics include:
- Loss of physiological reserve
- Cellular and metabolic derangement
- Rapid and unpredictable deterioration
Organ dysfunction may manifest as:
- Hypotension or septic shock
- Acute kidney injury
- Altered mental state
- Hypoxia or respiratory failure
- Coagulopathy or metabolic acidosis
Clinically and legally, sepsis is distinct from infection not because of the pathogen involved, but because of the consequences of the host response.
Core Clinical Differences
The medico-legal distinction rests on the recognition of deterioration rather than the initial diagnosis.
Infection
- Stable observations
- Preserved organ function
- Predictable course
- Routine management appropriate
Sepsis
- Physiological instability
- New or worsening organ dysfunction
- Time-critical emergency
- Requires urgent escalation and treatment
In negligence claims, the central issue is often whether clinicians failed to recognise that infection had progressed to sepsis and failed to act accordingly.
Red Flags and Escalation Duties
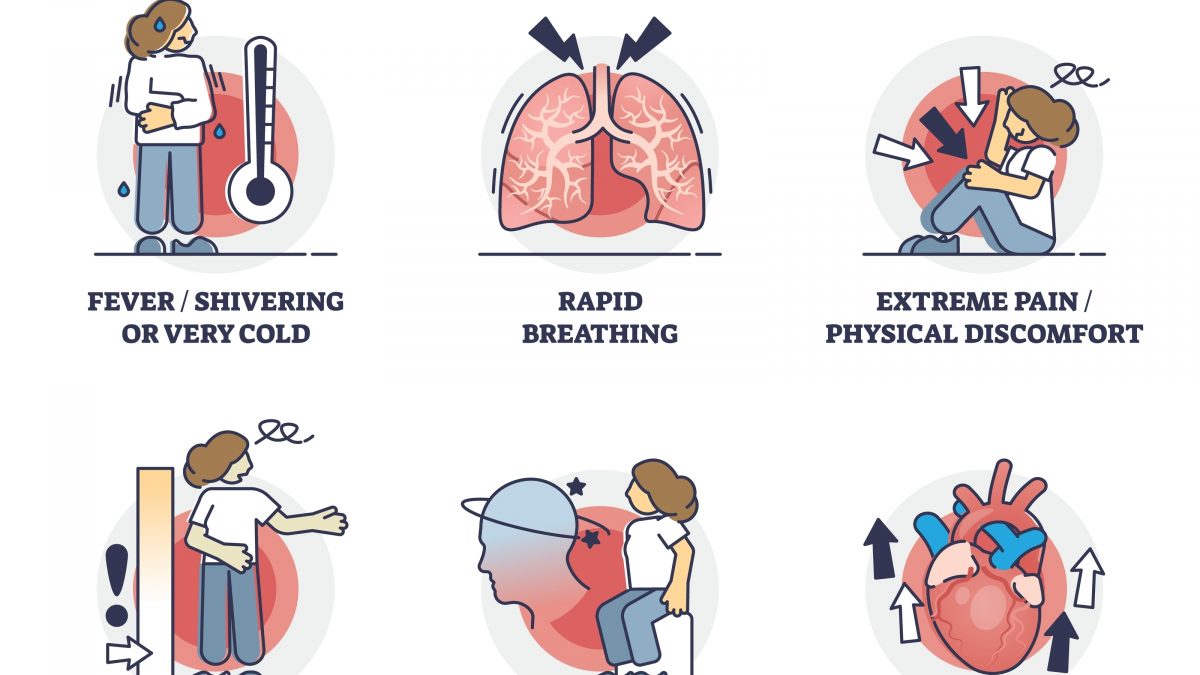
Claims frequently focus on missed warning signs and delayed response. Red flags suggesting sepsis include:
- New confusion or reduced consciousness
- Persistent tachycardia or hypotension
- Tachypnoea or hypoxia
- Oliguria or rising creatinine
- Elevated lactate
- Failure to improve with initial treatment
From a medico-legal standpoint, documentation demonstrating awareness, reassessment, and escalation in response to these features is critical.
Case Law and Medico-Legal Precedent
There is no single reported appellate judgment in UK law that expressly defines or contrasts infection and sepsis as distinct legal concepts. However, this does not diminish the legal significance of the distinction.
In practice, the difference is well established through clinical negligence claims and settlements, coroners’ inquests and Prevention of Future Deaths reports and expert evidence accepted by courts
Many sepsis cases resolve without a reported judgment, but the consistent pattern is clear: infection is not usually actionable. Failure to recognise and treat sepsis often is.
Claims for compensation commonly allege a failure to identify sepsis, a delay in senior review or escalation, a delay in antibiotic administration or inadequate monitoring or safety-netting
Courts assess these cases using established negligence principles: whether a reasonably competent clinician, given the information available at the time, should have suspected sepsis and acted differently. Importantly, sepsis remains a diagnosis of clinical judgement, not one dependent solely on scoring systems or rigid criteria.
Inquests and Public Law Implications
Coroners’ findings frequently reinforce the distinction, identifying missed opportunities where early sepsis indicators were treated as benign infection. These findings, while not determinative of civil liability, strongly influence clinical standards, policy development, and regulatory expectations.
Conclusion
Infection and sepsis lie on a clinical continuum, but they are not interchangeable terms. Infection describes the presence of pathogenic organisms; sepsis describes a catastrophic failure of the host response leading to organ dysfunction and death if untreated.
For clinicians, the challenge is timely recognition of deterioration. For medico-legal professionals, the key question is whether warning signs were recognised, interpreted, documented, and acted upon. Although no single case defines the distinction in law, the body of clinical negligence practice overwhelmingly supports its central importance in determining breach of duty and causation.