
Foreign Bodies in the Eye: what is the extent of injury?
10th August 2020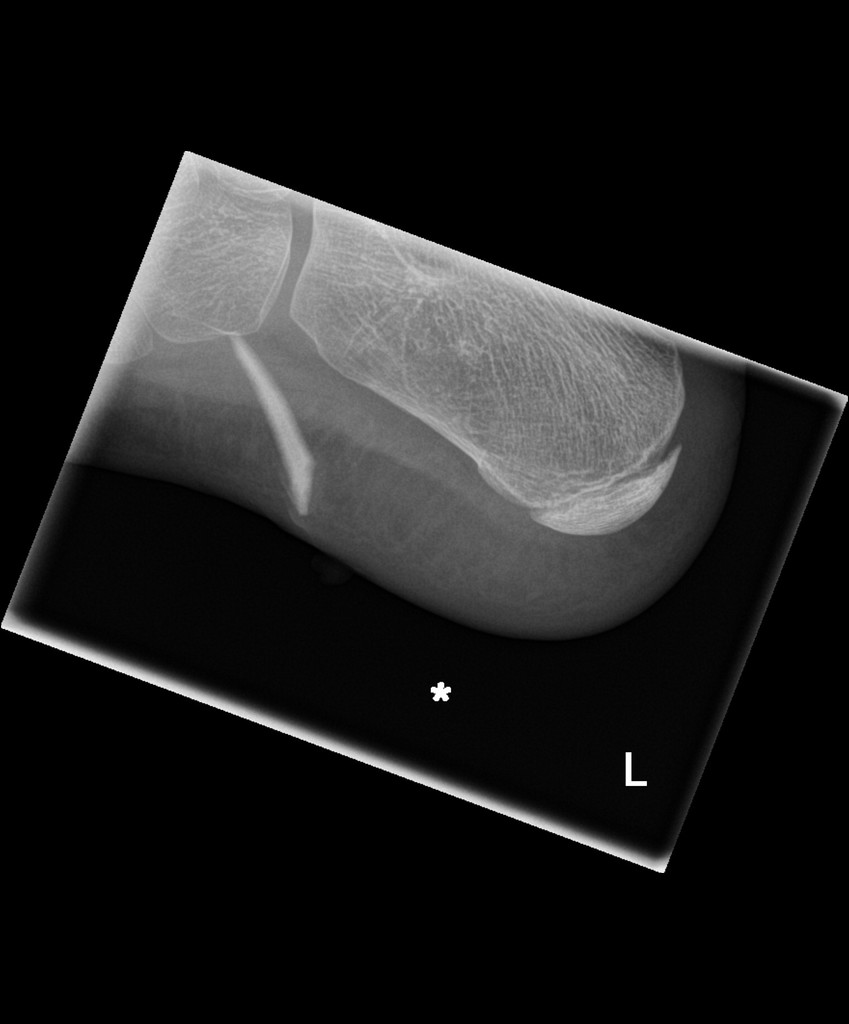
Foreign bodies in the skin: identification, exploration and removal
26th August 2020Hand injuries are rarely life-threatening, but they can lead to significant, life-altering complications. They also make up about 5% of Emergency Department attendances. Injuries to the tendons or nerves in the hand can lead to permanent disability if not treated and referred accordingly. The responsibility lies on the emergency department physician to identify time-sensitive, limb-threatening injuries, obtain detailed clinical information, and facilitate treatment and follow-up. (Bowen & Slaven, 2014)
Several retrospective studies have shown that missed or delayed hand injury diagnoses pose a significant medicolegal risk often to the Emergency Department. For example, a 2010 retrospective review by Brown et al found that out of 11,529 closed malpractice claims in the United States from 1985 to 2007, open finger injuries were in the top 10 most common diagnoses resulting in medical malpractice litigation.
The hand is anatomically complex, which is why fractures and other injuries can be easy to miss, even with radiographs. (See my past article on scaphoid fractures.) This underscores the importance of a clinician’s physical examination skills and the ability to obtain a thorough medical history.
Tendon injuries are the second most common injury in the hand; usually caused by a penetrating injury. They can result in severe functional loss if not repaired. Nerve injuries in the hand are, relatively-speaking, less common than tendon injuries, however, they can also result in loss of function. Early intervention provides the highest chances of recovery. (BSSH)
A good understanding of the mechanism of injury (blunt force, penetrating force, high pressure injection, etc.) will provide valuable information on the possible types and extent of injury the patient has suffered.
Once the history is obtained the subsequent physical examination should include visual observation and testing for sensation and motor assessments before any local anesthetic is administered. Loss or alteration of sensation may indicate injury to the median, ulnar, radial nerves or the digital nerves.
The integrity of all tendons should also be established separately by testing the patient’s ability to flex against resistance. If resistance is absent or reduced, or the level of pain is so high as to prevent the patient from flexing, it is likely that a tendon injury is present. Knowing how to test for the profundus and superficialis tendons of the fingers separately is a skill that all Emergency Medicine doctors should learn.
The majority of acute tendon or nerve injuries require re-evaluation by a hand surgeon. In these cases, the recommended course of action is to splint the affected joint, and if a penetrating injury is present, to stitch the wound with non-absorbable sutures. The patient should be referred to a hand surgeon within 7 days. A rapid referral is essential since some injuries, such as a flexor tendon injury, become irreparable after 7-10 days. (AFP)
In some cases, the rupture in the tendon may be partial, which could still allow the patient some flexing ability. This may make the tendon injury harder to diagnose. Missing this injury can lead to a full tear in the tendon if the patient is allowed to leave without adequate treatment. (Schoffl et al, 2012)
Some types of hand injuries require immediate surgical intervention. The need for thorough clinical diagnosis skills is especially evident in cases of high-pressure injection injuries. These may appear benign and painless at first, but the delay of treatment causes an exponential increase in subcutaneous damage that can lead to loss of function or risk of amputation. (Verhoeven & Hierner, 2008)
The main takeaway here is that an ED physician must have adequate knowledge of the anatomy of the hand and be aware of the clinical signs that point to high-risk and time-sensitive injuries. Acting quickly and methodically will protect the patient from limb-threatening complications and ensure that the physician is protected against future litigation because they have met the standard of care.





3 Comments
[…] the low density of the cartilage that makes up the growth plates. Another consideration is that an injury to an adult that might result in a sprain or joint dislocation often results in a fracture to a child. […]
[…] of the assessment in the Emergency Department is for the assessing clinician to take an accurate history of the mechanism of injury. Treatment of the visible injury is less important than recognising the potential chemical […]
[…] causes of tenosynovitis with De Quervain’s are often not clear. Overuse of the thumb tendons, particularly through repetitive actions, is often a causal factor, as is a […]